ABSTRACT
A patient with Graves' disease was admitted with a thyroid storm. She had severe hypercalcaemia caused by thyrotoxicosis. Treatment was complicated by vomiting and diarrhoea. With intravenous ondansetron, hydration and bisphosphonates, GI symptoms improved and oral thyreostatics could be started. This, combined with bisphosphonate administration, resulted in a mild hungry bone syndrome.
LEARNING POINTS
- Thyroid storm is an endocrine emergency with high mortality which needs prompt treatment.
- Thyrotoxicosis can increase calcium levels due to several mechanisms.
- When gastrointestinal symptoms are complicating treatment, intravenous ondansetron can be used to facilitate oral treatment.
KEYWORDS
Endocrinology, thyrotoxicosis, hypercalcaemia, pharmacology, bone disease, hungry bone syndrome
INTRODUCTION
Hypercalcaemia has several known causes, but primary hyperparathyroidism and malignancy-associated causes account for 90%[1]. 16%–23% of patients with hyperthyroidism have hypercalcaemia, but this is usually mild and asymptomatic[2]. A calcium concentration as high as in this case has been described only once before[3].
Treatment of a thyroid storm should be started promptly but can be difficult when patients have gastrointestinal complaints. Hypercalcaemia as a result of high bone turnover can aggravate gastrointestinal symptoms. Clinicians should be aware of the limited availability of parenteral treatment options and alternative strategies in this acute situation.
CASE REPORT
A 36-year-old woman had recently been diagnosed with Graves' disease. Treatment was postponed because she was breastfeeding. She presented at the emergency department with complaints of severe diarrhoea, a fever, tremor, nausea and vomiting.
On physical examination, we saw a thin, weak woman with a temperature of 38.6°C and a tachycardia of 114 beats/min. Further physical examination revealed a mildly enlarged thyroid gland but was otherwise unremarkable. There were no signs of Graves' ophthalmopathy.
The laboratory results showed a thyroid-stimulating hormone (TSH) of <0.01 mU/l, free T4 of >100 pmol/l and calcium level of 3.53 mmol/l (Table 1).
| Normal values | On admission, 19 July | 20 July | 23 July | 27 July | 7 August | |
|---|---|---|---|---|---|---|
| Hb (mmol/l) | 7.8-9.6 | 7.7 | 7.8 | |||
| MCV (fl) | 80-100 | 81 | ||||
| Leukocytes (x 109/l) | 4.5-10.0 | 9.6 | ||||
| Thrombocytes (x 109/l) | 150-400 | 249 | ||||
| Sodium (mmol/l) | 132-145 | 136 | 138 | |||
| Potassium (mmol/l) | 3.4-4.5 | 3.9 | 3.1 | 4.4 | ||
| Creatinine (mmol/l) | 44-80 | 44 | 43 | 44 | ||
| Urea (mmol/l) | <8.0 | 3.7 | 2.2 | 4.8 | ||
| Calcium (mmol/l) | 2.15-2.55 | 3.51 | 2.99 | 1.84 | 2.02 | 2.35 |
| Phosphate (mmol/l) | 0.80-1.40 | 0.63 | 1.08 | |||
| Albumin (g/l) | 35-52 | 39 | 30 | 35 | 40 | |
| ASAT (U/l) | <30 | 28 | ||||
| ALAT (U/l) | <35 | 47 | ||||
| Alkalic phosphatase (U/l) | <120 | 100 | ||||
| Lactate dehydrogenase (U/l) | <250 | 409 | ||||
| Amylase (U/l) | <100 | 171 | 106 | |||
| CRP (mg/l) | <5.0 | 5.3 | 12 | |||
| TSH (mlU/l) | 0.30-3.7 | <0.01 | <0.01 | |||
| fT4 (pmol/l) | 12-21 | >100 | 38 | 9.0 | ||
| T3 (nmol/l) | 1.2-2.8 | 4.8 | 1.3 | 1.4 | ||
| PTH (pmol/l) | 1.60-6.90 | 0.54 | ||||
| Vitamin D (pmol/l) | 47.0-130.3 | 155.5 |
Table 1 - Laboratory values
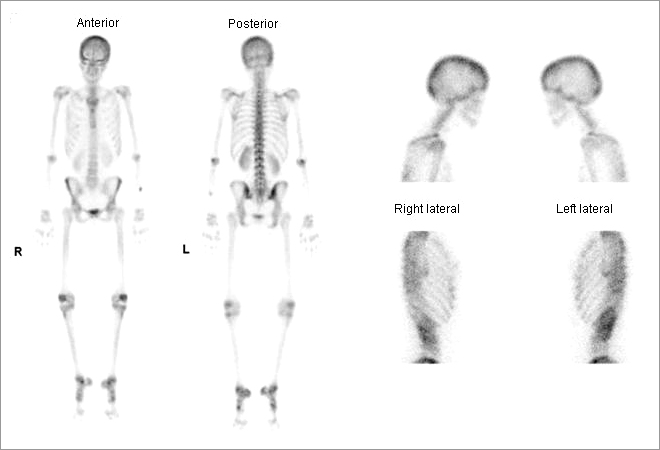
She was diagnosed with a thyroid storm and a severe symptomatic hypercalcaemia and admitted to our hospital. Parathyroid hormone (PTH) was low, and a bone scan showed a diffuse increase in bone remodelling (Fig. 1).
Because of severe vomiting, we prescribed intravenous propylthiouracil (PTU) 200 mg q.i.d., beta blockade and Lugol's solution 1 ml t.i.d. However, our hospital pharmacist informed us that non-oral formulations of thionamides are not commercially available in the Netherlands. Given the acute nature and severity of disease, compounding the medication was not a viable option.
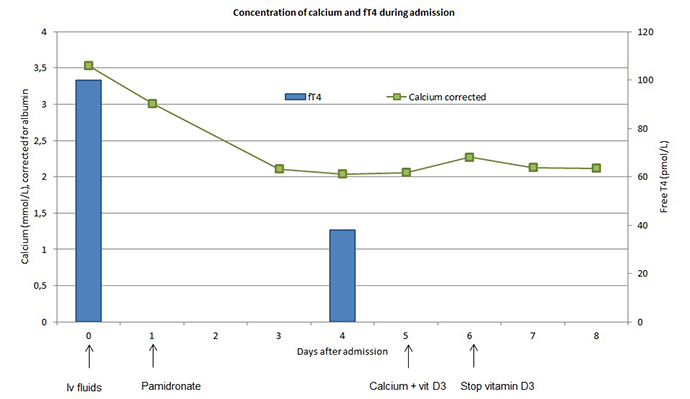
We decided to treat vomiting with intravenous ondansetron 4 mg q.i.d. Hypercalcaemia was treated with hydration and pamidronate. Vomiting diminished and oral thionamide and Lugol's solution could be started. Hungry bone syndrome was expected, and four days after admission our patient developed hypocalcaemia. We prescribed calcium and vitamin D, which increased the calcium to normal values (Fig. 2). Eight days after admission, the patient could be discharged in significantly improved condition.
DISCUSSION
Signs and symptoms of thyrotoxicosis are due to increased metabolic rate and include hyperactivity, irritability, palpitations, diarrhoea and vomiting. Without treatment, mortality of Graves' disease is 10%–30%[1]. With treatment, the prognosis is good. In its most severe form, it can present as a “thyroid storm”, with a mortality of 20%–30%[4].
Symptoms of hypercalcaemia include fatigue, nausea, vomiting and cardiac arrhythmias[1]. In this case, both thyrotoxicosis and hypercalcaemia could cause gastrointestinal complaints.
Thyrotoxicosis causes hypercalcaemia by an increase in both the number and activity of osteoclasts[5], and increases the responsiveness of osteoclasts to PTH[6]. It also causes high circulating IL-6 levels, stimulating osteoclastogenesis[7]. The severity of hyperthyroidism correlates positively with the rate of bone resorption[7].
Although serum calcium is often increased, net calcium balance is negative due to an increased calcium excretion[8]. Compensatory hypoparathyroidism and low levels of active vitamin D are usually found[7,9]. This patient had a slightly elevated concentration of vitamin D, but not enough to significantly increase calcium.
The increased bone turnover in thyrotoxicosis, shown in the bone scan in Fig. 1, causes decreased bone mineral density and an increased fracture risk[10].
Because thyroid storms have high mortality rates, treatment should be started without delay[11]. Prevention of synthesis of new T4 and T3 can be achieved by thionamides. As soon as, and only after, synthesis is suppressed, inorganic iodine should be given to block thyroid hormone release. Beta blockers are required to control the cardiovascular symptoms of the thyroid storm.
An elevated calcium level can lead to neurologic complications and cardiac arrhythmias. Treatment of thyrotoxicosis with thionamides is expected to lower the rate of bone turnover and therefore gradually decrease the serum calcium level in days to weeks[12]. However, due to the severity of symptoms, we felt that we could not wait for this. In addition to hydration with intravenous fluids, we decided to treat with pamidronate because its calcium-lowering effect starts within 24 hours.
Four days after admission, hypocalcaemia developed, which we attributed to hungry bone syndrome. This condition is most commonly seen after parathyroidectomy[13]. When treatment for thyrotoxicosis is initiated, bone formation starts again, leading to an increased uptake of calcium in bone[14]. This effect was probably aggravated by the bisphosphonate. With replenishment of calcium and vitamin D the serum calcium levels in our patient normalized.
Treatment of thyrotoxicosis was further complicated by vomiting, which could have been caused by both hypercalcaemia and thyrotoxicosis. Rectal, sublingual and intravenous preparations of both PTU and inorganic iodine have been compounded and used successfully in a few cases[15]. However, parenteral formulations of inorganic iodine or PTU are not commercially available in the Netherlands. Rectal preparations were unsuitable for use in our patient because of severe diarrhoea.
We successfully treated vomiting with ondansetron. To our knowledge, the effective use of ondansetron for vomiting in thyroid storm with hypercalcaemia has not been described before.
CONCLUSION
Thyrotoxicosis is a rare cause of severe symptomatic hypercalcaemia. Vomiting and diarrhoea can complicate treatment because parenteral formulations of thyreostatics are not commercially available in several countries, including the Netherlands. However, intravenous ondansetron seems efficacious in treating vomiting in thyroid storm, thus facilitating oral administration of thyreostatics. Hypercalcaemia in thyroid storm can be corrected by hydration, thyreostatic treatment and beta blockade. Especially if bone resorption is inhibited using a bisphosphonate, hungry bone syndrome must be anticipated and treated accordingly, since thyrotoxicosis induces a net calcium deficit.